Exclusive Interview on COVID-19 with SARS Veteran Dr. Sarah Borwein (Updated)
18th April 2023
There is currently an explosion of information, comments and opinions on COVID-19 on the internet and social media. We believe that on serious topics in general, and on public health matters in particular, it is essential that you rely on facts and credible, expert information. Our mission at Alea remains to bring you the best possible information and advice, so you can make the best choices for you and your family.
Alea is proud to bring you an exclusive interview with SARS Veteran, Dr. Sarah Borwein, to share unique insights on the novel coronavirus (COVID-19).
We couldn’t think of a better person than Dr. Sarah Borwein. Originally from Canada, Dr. Borwein has been practicing in Hong Kong for over 15 years, and prior to that successfully ran the Infection Control program for the only expatriate hospital in Beijing during the SARS period. Dr. Borwein is also a mother of 3, and has been helping families in situations including epidemics in Asia since 2001.
What would you say are the main differences between COVID-19 and SARS?
COVID-19 and SARS do share some common features: they belong to the same family of viruses, they both seem to have jumped from animals to humans, they both likely originated in China and both can cause severe pneumonia.
There are some important differences, however. SARS was more lethal than COVID-19, but less easily transmitted. It went straight for the lungs and caused severe pneumonia which became transmissible only when patients were quite severely ill and usually by then in the hospital. Overall, about 10% died.
COVID-19, on the other hand, is more likely to replicate initially in the upper respiratory tract, with the result that some individuals may shed a lot of viruses when they are only mildly symptomatic. It’s thought that at least some unknown percentage of people never get symptoms. But of the ones who do get sick, about 20% get severely ill and need to be hospitalized. Death rates vary a lot by age, underlying illness and access to care but overall are thought to be less than 1%.
So COVID-19 is a lot less lethal than SARS, but harder to control because it spreads more easily and by people with milder (or no) symptoms. That’s why, despite being considerably less likely to kill you than SARS was, COVID-19 has in total killed far more people in 16 weeks than SARS did in 8 months.
Another important difference is that medicine has advanced considerably in the 17 years since SARS. In 2003, it took months to identify the virus and develop a test. For COVID-19 that happened within a couple of weeks.
During SARS, high-dose steroid treatment was used extensively in an attempt to dampen down the damaging immune response to the virus. This turned out to cause more harm than good and has been abandoned this time around. Instead, new treatments are proving useful, such as some HIV drugs that also are active against coronaviruses, and most famously, the anti-malaria drug Chloroquine. The jury is still out on how effective these treatments are, and it should be noted that they do have significant side effects and shouldn’t be taken without supervision. Newer antivirals such as Remdesivir, and various other treatments are being trialed and more than 30 candidate vaccines are on the horizon.
All of the vaccine possibilities are pre-clinical though, meaning that even those that are ready to test have to go through a series of trials for safety and efficacy, a process that will take more than a year. And that’s moving at warp speed compared to the usual 5 to 15-year process.
Ultimately a vaccine and/or an effective treatment — preferably both — will likely be the answer to taming this virus and preventing it from being a threat to us.
Which lessons can be learned from SARS to best manage the current outbreak?
The most important thing we learned in SARS was that infectious diseases do not respect borders or government edicts, and cannot be hidden. It requires international cooperation, transparency and sharing of information to control an epidemic. This epidemic will underscore that message, but I wonder if another takeaway won’t be that the international community has to get in sync in the management of global infectious disease threats. We still like to think of diseases as other countries’ problems right up to the moment when they land on our own doorstep. This pandemic has shown us that that is often too late.
We also learned the importance of providing good, balanced, reliable information to the public. In any epidemic, there is the outbreak of disease and then there is the epidemic of panic. And nowadays, there is also what the WHO has termed the Infodemic, the explosion of internet information about the epidemic. Some of it is good information, but some of it is rumor, myth, speculation and conspiracy theory, and those things feed the anxiety. It can be hard to sort out which information to believe, so it is important to choose trustworthy sources. Panic and misinformation make controlling the outbreak more difficult. So does complacency.
A very important lesson learned in areas that experienced serious SARS outbreaks was that it takes a village to control a virulent infectious disease. In this situation, personal autonomy has to give way to community welfare. None of us is safe unless we are all safe, so every individual needs to do their part.
Finally, SARS was the first time we realized that respiratory illness could be spread to healthcare workers. When the SARS epidemic started in 2003, the hospital I worked at had two N95 masks, in case of the occasional case of active tuberculosis. Many people had never even heard of an N95 mask! Now we recognize that healthcare workers, the very people we depend on to help us if we get sick, are at particular risk. It is clear that if we fail to provide healthcare workers with adequate protection, they do become infected. COVID-19 puts frontline caregivers in hospitals in real danger, and special care has to be taken to safeguard them.
How serious is the situation now in Hong Kong compared to other places?
So much has changed since I last updated this article. The epicenter has moved from China to Europe, the United Kingdom, the United States, and beyond. Hong Kong’s initial success in containing Coronavirus has been threatened by the second wave of imported cases from these places.
Cases numbers in Hong Kong increased from fewer than 150 in early March to nearly 1,000 by Easter. In response, Hong Kong took aggressive measures, basically shutting down international arrivals and enforcing mandatory testing and quarantine for all those who do enter, as well as more stringent social distancing measures, a ban on public gatherings of more than 4 people and closing many venues such as bars and sports clubs. The new case numbers have started to decline again. Fingers crossed, but perhaps we are gaining some control over this second wave. It is too early, however, to relax our guard, as it will take a few weeks to be sure there isn’t disease percolating quietly in the community.
Our second wave was largely unleashed by returning Hong Kongers and expatriates coming home. In part, this was because they felt safer here, due to Hong Kong’s initial success in managing the epidemic. This has caused some problems, but is also a testament to the fact that there are benefits to being in a place that not only has the know-how and resolution, but also has been tested before.
Lessons from Hong Kong and Asia
Several lessons are emerging from the experience of Hong Kong and other Asian countries. The first lesson is “Go hard, and go early”. How things might have been different if some other places had done what we did and instituted vigorous measures since January when there were only a very few cases or none? Hong Kong response started before we had any cases at all, and kicked into high gear when we had only 5. Singapore, Taiwan, Macao, Thailand, Vietnam and South Korea did the same.
When started early, countries can contact trace every case and try to contain or eliminate the disease completely by isolating infected individuals quickly, and quarantining their contacts before they can spread the infection. Hong Kong’s impressive contact-tracing work has helped define where the local cases are coming from, so that measures can be taken to curb community spread. As a result, even though life is not normal, we are not in complete lockdown. Countries that didn’t start taking COVID-19 seriously until they had a great many cases cannot do this. Extreme social distancing is the only tool then available; this will help reduce the impact of the disease, preventing a worst-case scenario, but a lot more people will still get sick and die than here, and the economic consequences may be much direr.
We’ve also found that quarantine and isolation must be strictly enforced n order to be effective, and unfortunately, this requires intrusive measures including tracking bracelets, fines and even jail terms. Without these, it’s far too easy for people to find reasons why they personally are different or exempt.
Community engagement is vitally important. Hong Kong people lived through SARS and understand at a visceral level how important it is to practice social distancing, wear masks, wash their hands and listen to public health advice. This epidemic happened on the back of months of civil unrest that left us with a weakened and unpopular local government. That could have been disastrous. But we do have highly respected public health authorities and infectious disease specialists, many of whom are seen as SARS heroes. Both the government and even more importantly the local population, do listen to their advice. SARS taught us that our own health is dependent on the health of the whole community, and that lesson has not been forgotten.
It all seems eerily familiar, but also oddly comforting in a “we got this” kind of way. We know how to do this. Hong Kongers seem to have just dusted off their old SARS habits and gotten on it, a bit like riding a long-unused bicycle.
What have we learned about the disease?
Symptoms of COVID-19 typically appear 2 to 14 days after exposure. Unlike the flu, COVID-19 often starts slowly with some combination of mild symptoms such as:
- low-grade fevers
- sore throat
- muscle aches
- dry cough
- headache
- diarrhea
- nausea
- loss of taste and smell
Not all patients have a fever and not all symptoms need to be present. Loss of taste and smell does not happen in all cases but is quite specific when it does.
For most patients, the disease never progresses further; these symptoms persist for about 2 weeks and then resolve. For up to 20%, however, there is progression to pneumonia, usually in the second week, with shortness of breath, chest pain or chest tightness, and sometimes high fevers. A smaller percentage will become critically ill and require breathing support. The overall death rate is highly dependent on access to care. When good care is available, it is probably under 1%.
Any number of deaths is too many, and even a death rate of 1% is many times that of the flu. But the really crucial thing about this disease, and the reason we should all take it seriously no matter our age, is not so much the death rate, but the significant rate of severe disease (up to 20%) requiring hospital care. This means that without control measures, or with control measures imposed late, that health systems can be rapidly overwhelmed by very sick patients.
Risk factors for severe disease are advancing age, diabetes, heart disease, hypertension, lung problems including asthma, and cancer. Smoking and obesity may also predispose to a worse outcome. Men seem to be more at risk than women. These are risk factors only; we have seen centenarians survive Coronavirus while some young healthy people have succumbed.
Children and teens are not immune to COVID-19. They can become infected but it’s less common for them to become seriously ill. They can, however, pass the disease to others who are more vulnerable to severe outcomes.
Which precautions are the most critical to stay safe?
DO wear a mask (see below),
DO wash your hands regularly. Alcohol-based hand sanitizer is an acceptable alternative, except when your hands are visibly soiled.
DO avoid crowds, and keep at least 6 feet away from other people, especially those with fever or cough.
DO practice social distancing. It’s becoming apparent that COVID-19 is a clustering disease. It spreads, for example, at meetings and conferences, on cruise ships, in bars and Karaoke clubs, at food-sharing events, in old age homes, in households, and at religious gatherings. While it’s not entirely clear what the mechanism of transmission is in these settings, it underlines the importance of social distancing measures. Stay home as much as possible.
DO get enough sleep, eat well, and get some exercise. In other words, look after your general health.
DO listen to local public health advice.
DON’T smoke (not even pot!) or vape; this damages your lungs and makes you more susceptible to severe disease.
DON’T travel, go to work or socialize when you are feeling unwell yourself. It won’t be appreciated!
The great mask debate: how important is it to wear one?
The mask issue has created a lot of confusion. My own view on this has changed as the epidemic has progressed. In the early days, I too, was tempted to listen to the advice from some authorities that masks are not helpful for the general population. I don’t like wearing a mask all the time any more than any of you and it seemed to be the prevailing expert opinion that they weren’t that helpful. However, it has become increasingly obvious that masks ARE an important part of the prevention package, something the Hong Kong authorities have always advocated.
COVID-19 is spread by respiratory droplets that are coughed, sneezed or talked out by infected people (droplet spread). It can also be spread when these infected droplets fall onto surfaces that are then touched by susceptible people who then touch their nose, eyes or mouth (contact spread). Plain surgical masks provide some protection against droplet spread infections. It’s hard to quantify how much, but even if the protection is only 10-20% that's worth having, when combined with good hand hygiene and social distancing. Even more than that, this is an infection that can be spread when asymptomatic or pre-symptomatic, and we know that masks do significantly help to prevent infected people from transmitting to others or contaminating nearby objects. Everyone should consider themselves potentially infectious and wear a mask to protect others.
Wearing a mask when around others is a civic responsibility and an act of solidarity: I wear a mask to protect you, you wear a mask to protect me. Everyone is protected if we all do it.
But when the epidemic ends, please stop wearing masks. They stop us from smiling at each other.
Conflicting public health advice
It’s not just the advice about masks. Many people are confused by the differing advice and policies in different countries regarding sheltering at home, getting tested and the need for isolation and quarantine. For expatriates, they may be hearing one kind of advice from their home country and another from Hong Kong’s Department of Health. You don’t get to choose which advice you like better! It’s important to listen to public health advice from where you are living.
These differences arise because Hong Kong and several other Asian countries have been able to contain the coronavirus outbreak, whereas European countries and North America are just trying to mitigate it to reduce the death toll. In a containment context, we rely not just on social distancing and wearing masks, but also on case-finding (testing every symptomatic person), tracing their contacts, isolating in hospital people who have the disease (no matter how mild a case), and quarantining those at risk.
Countries that cannot contain the epidemic at this point have too many cases to contact trace or even test, and can only accommodate the most severe cases in hospital. So yes, they ask people with milder symptoms to stay at home and can’t possibly quarantine contacts. This is the approach that has to be adopted when countries are too late in their response to be able to attempt containment. While it may seem preferable for some to stay at home if they have only mild symptoms, the Hong Kong policy is better both for you (early treatment helps), for the community, and in previous pandemics, resulted in faster economic recovery. Countries relying on mitigation will have many more deaths than Hong Kong and a longer and more stringent lockdown will be required.
Conflicting public health advice has also given some people the idea that if they aren’t elderly and infirm, they won’t have severe disease and don’t need to bother getting tested or treated. In the rush to reassure people and persuade them to stay home rather than flooding over-stretched hospitals, the message has somehow been conveyed that younger people are not at risk. This is simply not the case. 35%f of ICU cases in Hong Kong are under the age of 50, for example, and many have no underlying health issues. Age and other health conditions do increase your risk, but youth and good health do not guarantee you a mild case. It’s true that most young, healthy people will recover from even a severe case, but only when they have access to care from a system that can cope with the numbers. It’s a virus that deserves respect.
Hong Kong’s experience has been that early treatment, preferably in the first week of illness when symptoms are still mild, is important and prevents progression to needing intensive care. That’s why people living in Hong Kong should get tested early and cooperate with the treatment and isolation protocols. Consider yourself fortunate if this is available to you. Hong Kong has ICU admission rates under 2.5% and has had only 4 deaths.
If you are in a place where the outbreak is more serious, this is also why you should be diligent about following social distancing advice and avoid getting sick.
Flattening the curve
The main objectives of social distancing policies are to avoid an epidemic peak that overwhelms healthcare systems, flattening the epidemic curve while we wait for vaccine development and effective antiviral treatments. This little graph explains the importance of slowing down the outbreak:
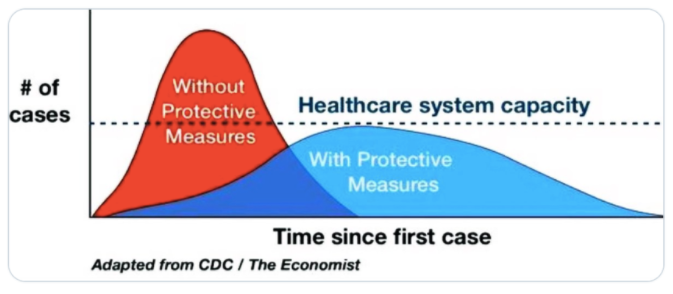
With mitigation measures, the peak and speed of the epidemic are slowed enough that capacity is not over-run. Without them, the healthcare system has great difficulty coping with the sheer number of sick people. When healthcare systems get overwhelmed, people die because they can’t access care for severe Coronavirus disease. And they die because hospitals are too over-stretched to provide care for other medical problems that continue to happen.
A few weeks ago, I might have said this was catastrophizing. But we are seeing it happen right now in first-world countries, like Italy, France, Spain and the US.
When healthcare systems are overwhelmed, the fatality rate goes up by at least ten-fold.
That’s why it’s so important to slow this virus down.
If you live in Hong Kong, follow the advice of the local public health authorities. They have been impressively successful at keeping the epidemic, not just within healthcare capacity, but contained.
If you live elsewhere follow the advice of the country you live in. It may be more appropriate to the local situation, where mitigation may be the main goal.
How important is testing?
Testing is another area where there is a lot of noise and little practical advice. Some kinds of testing are most useful on a population level, to understand the extent of disease. Others are better for the diagnosis of individuals.
The first kind of test is an RT- PCR test, which uses molecular genetic technology to look for the RNA (genetic material) of the virus. This is the usual best test in people with symptoms. The 2 most important things to know about RT-PCR testing are that it is most helpful when it is positive, and that it is not very helpful in general in people who have no symptoms.
RT-PCR testing has a high rate of false-negative results, up to 30%. Quite a number of COVID-19 patients have needed to be tested several times before the test becomes positive. People with no symptoms are especially likely to have a false-negative result.
The second kind of test is a serology test, which is a blood test to look for antibodies, the body’s response to the infection. The role of serological testing is still being defined. It is most helpful for population screening (serosurveys). It is also useful in people with negative RT-PCR but ongoing symptoms suggestive of COVID-19. Serology becomes positive about 5 to 8 days on average after illness onset, too late for use in early diagnosis.
For either test, mass screening is the only circumstance in which testing is widely useful in people with no symptoms. Serosurveys will be helpful in determining the percentage of the population that has been infected and in understanding the spectrum of disease.
There is a lot of wishful thinking about the role of serology in getting us “back to normal”. There is still too much we do not yet know about the antibody response to COVID-19, how long it lasts, or how well it protects against re-infection. The WHO recommends that serology tests not be used yet for clinical decision-making. In Hong Kong, at this point, a positive serology test may land you in hospital for several days, in order to rule out acute COVID-19.
Save time, money & worries on your insurance. Contact us!
What are the questions you hear the most from your patients?
The most common questions I now hear are “how worried should I be?” and “how long will this last?”
The answer to the first question is that you should not worry, but should have an appropriate level of concern. Most people who contract Coronavirus will recover and be just fine. But it is not a disease to take lightly. You should be worried enough to take the appropriate measures to help stop its spread. Even if you don’t get very sick yourself, you may infect someone else who does. Every individual’s actions matter.
And from a public health point of view this is an urgent situation. A highly transmissible disease, even with low fatality rates, can cause huge disruption and can actually end up killing more people than a less contagious disease with higher case fatality rates. We’ve seen that happen repeatedly even in first-world countries like Italy, Spain, the UK and the US. That’s why so much effort is being made to stop or at least curb it.
In terms of how long this will last, I really don’t know. Viruses are notoriously unpredictable. We can only work with modeling estimates, and those suggest that we may have to deal with cycles of disease for up to 18 months or more. That does not mean 18 months of complete shutdown. One writer, Thomas Peuyo, has referred to the Hammer and the Dance. During periods of disease resurgence, strict measures need to be applied (the Hammer). These could be somewhat relaxed (the Dance) when disease levels are lower. During the intervals of relaxation, we would rely on rapid testing, isolation and quarantine coupled with less restrictive social distancing measures.
In other words, we may cycle between the Hammer and the Dance for a year or two, until we have a vaccine or effective treatments, or both. We may have to get used to a “new normal” for some time to come.
That said, modeling provides only a guess-timate. Predictions can change dramatically if underlying assumptions are a little bit off, if social distancing measures are more or less effective, or if the virus decides to behave differently.
The only thing I know for sure, is that this WILL pass. Everything else is conjecture.
Which psychological impacts do you see so far on the community in Hong Kong?
The mental health effects of this outbreak are serious. School closures, cancellation of many events, working from home, isolation, economic loss and the uncertainty about how and when this will end are creating an atmosphere of fear and sadness that is taking a toll on many people. Especially coming on the heels of the months of protests we had beforehand.
It’s normal to experience stress and a certain amount of sadness in response to the very serious precautions that we all need to take and the things we're temporarily losing out on in the process. It's important to note that even though we're all in this together, a person's response may be very individual. A large part of anyone's reaction to the COVID-19 pandemic will depend on their personal vulnerabilities that predate this crisis.
While there are some people who are overly concerned and panic-stricken, there are others who choose not to follow public health directives, and who might benefit from having more anxiety at the moment. There are also those who worry more about isolation and quarantine than about the disease itself. This is not rational either. Isolation and quarantine will not kill you or make you seriously ill, Coronavirus might. Or might result in you infecting and killing someone else.
In the expatriate population in Hong Kong, there is a real possibility of parents being separated from their children due to illness. The local population for the most part has extended family who can step in if, for example parents are isolated in hospital and someone needs to accompany a child to quarantine. Expatriates who are far from their family supports do need to give some thought to who might do this in the event that both parents are sick.
How optimistic are you on this outbreak's future path and the ability of healthcare systems to contain it?
To a large extent, we are trying to predict the unknowable. This is a new virus with many uncertainties around it. It is possible that it will disappear like SARS did or dissipate when the seasons change. But it would be very foolish to count on that.
We have seen many countries be overwhelmed by a tidal wave of COVID illness and in these places some of the worst-case scenarios have played out. But elsewhere, including here, good preparedness and rapid action have been effective and shown us a way forward.
During the Spanish Flu pandemic of 1918-1919, the places that fared the best were the ones that took the disease seriously from the start, isolated sick people early, instituted comprehensive social distancing measures and continued public health measures until the epidemic was unquestionably under control. St. Louis, which did this, had half the death rate of Philadelphia, which did not. Economies also recovered more quickly in places that had taken decisive early action. In a series of natural experiments in which different places did these things to various degrees, the effectiveness of simple public health measures was proven over and over again.
Here in Hong Kong, we are fortunate to have one of the best public health systems in the world, strong epidemic planning and deep experience. Hong Kong took early and vigorous action and has a population that is disciplined in mitigation measures. Several authorities have singled out Hong Kong and Singapore as examples of places where COVID-19 has been well managed to date, stating that we provide hope and many lessons to other countries. We must not relax at this point; however. It’s important that we continue our stringent public health measures and cooperate with social distancing and other measures until the epidemic is truly over globally.
Any final advice to best manage this difficult period?
It may be early days to look for silver linings, and yet it is already apparent that there are some. Here are a few:
-
We’ve all learned lessons in better hygiene that may become lasting habits
-
There’s a new appreciation for the miracle of vaccination. If only we had one for COVID-19! The anti-vaxxers are very quiet right now.
-
We’ve been forced to slow down a little bit and appreciate stillness. In frenzied Hong Kong, that is something most of us have rarely experienced.
-
There is a myriad of new ways to catch up on culture, as Orchestras, Operas, Museums and others put their performances and exhibits online.
-
Similarly, online yoga routines and gym work-outs have proliferated, offering new ways to stay fit.
-
Pollution levels are drastically reduced. Even if this doesn’t last, it’s a reminder of what blue skies look like and that our economic model does not come without significant costs to the planet.
-
It may finally result in an end to the illegal wildlife trade.
-
Humans, when under pressure to do so, have a tremendous ability to innovate and problem solve. There will be some remarkable advances in technology, the biomedical sciences, and many other areas, not just because of research on Coronavirus, but also because we are being forced to do things differently.
-
Despite the difficulties of being cooped up for so long, and the conflicts that can create, many families and friends will also find that their shared memories of this intense and uncertain time will bind them together.
-
We have learned we are more adaptable than we think. Although ambient stress levels are high, we’ve seen people just getting on with what needs to be done. Home-schooling. Isolation. Cancellation of plans. Reduced income. We cope because we have to cope.
But most importantly, we have been reminded of our global connectedness and our essential humanity. Viruses don’t care about our race, our wealth or our social status. They pay no attention to borders, passports or politics. We are all in this together. One world, one fight.
We will be dealing with a storm raging around us, at varying levels of intensity, for some unknown period of time. The uncertainty is hard. The economic consequences are brutal. The rapidity with which many western countries have been overwhelmed is frightening. But this too shall pass.
The human spirit is resilient. Epidemics have shaped societies for centuries — consider the Black Death, Cholera, the Spanish Flu, HIV/AIDS and SARS. Our forefathers survived two World Wars in the past century. Economies recovered and life bloomed again afterwards. The new coronavirus will most probably be added to this list and become part of our collective memory as an event that changed the world.
Ironically, the more quickly public health measures succeed in controlling this Pandemic, the less we will appreciate them. We won’t see what was averted.
The epidemic won’t be over anywhere until is over everywhere. But it will be over one day, and it is the sum of our collective efforts that will determine how quickly that happens.
Meanwhile, Keep Calm, STAY HOME, and Wash Your Hands
Dr. Sarah Borwein is a Canadian-trained General Practitioner who co-founded the Central Health Group and has been practicing family medicine in Hong Kong for over 15 years. Dr. Borwein successfully ran the Infection Control program for the only expatriate hospital in Beijing during the SARS period and was also the lead communicator for the international community in Beijing at the time.
Save time, money & worries on your insurance. Contact us!
Looking for life or health insurance for yourself, your family or your team?
Do you already have an insurance policy? You could find a better plan!
Alea brings you choice, unbiased advice and outstanding service, with access to 100+ options from 25+ insurance companies. If you already have an insurance policy, switching insurance policies with Alea doesn’t cost you a thing.
Get free quotes with us today.
An advisor will be in touch to answer all your questions!
This article was independently written by Alea and is not sponsored. It is informative only and not intended to be a substitute for professional advice and should never be relied upon for specific advice.
